Case Studies
D4D currently has a portfolio of around 40 active projects across our clinical and cross-cutting themes. Since our inception we have been involved in over 120 projects across a wider range of clinical areas, resulting in more than 30 products that are either already available, CE marked, or close to market. A selection of examples of where our involvement has provided benefits during technology development, representing the breadth of activities and services that we are involved in, is presented below.
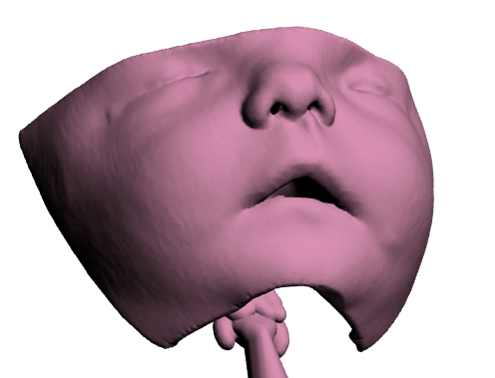
Paediatric Case Studies
TITCH
D4D works to improve quality of life for people with long-term conditions of all ages. As a consequence, our activities include managing the Technology Innovation Transforming Child Health (TITCH) Network. TITCH focuses on the identification of areas of unmet need where new technology could have an impact for child health, and also identifies where innovative technologies can lead to best clinical practice, and stimulates the adoption of these across the TITCH network.
For more information about the TITCH network click here or visit the dedicated website, here.
Starworks
The Starworks Innovation Project is a research collaboration to bring together children with prostheses and their families together with key opinion leaders from the NHS, industry, clinical academia, and leading national research centres with capabilities in child prosthetics. To visit the Starworks page on our website for more information click here.
For more information about the 10 proof of concept projects funded by Starworks, click here.
Perfect Patient Pathway Testbed
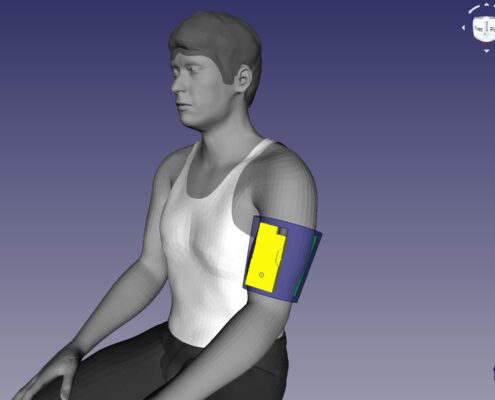
The Perfect Patient Pathway NHS England Wave 1 Test Bed programme was launched in January 2016 with the aim of benefitting patients with multiple long-term conditions through combining and integrating innovative digital technologies and service redesign, to keep patients well, independent and avoiding crisis points which often result in hospital admission, intensive rehabilitation and a high level of social care support.
The aims of the Test Beds programme were to create the conditions for testing ‘combinatorial innovation’ and improve patient outcomes and experience of care, at the same or lower cost than current practice, whilst supporting economic growth. More information about the NHS England Test Beds can be found here.
The Perfect Patient Pathway Test Bed programme also sought to build the infrastructure, and networks within the region, to test, refine and scale-up innovation; and to establish the effectiveness of this type of programme for identifying, implementing and evaluating the use of health technology in the NHS.
The programme objectives were to:
- Provide an ongoing platform for testing, refining and scaling-up innovations.
- Re-design pathways, bringing combinatorial technologies and system transformations to support holistic and personalised care.
- Support co-ordinated decision-making across health and care, informed by real-time data and predictive analytics.
- Evaluate the combination of new technologies and service re-designs producing robust and objective results that can be shared and disseminated.
- Embed the culture of transformation and improvement in NHS and other health and care organisations.
The Perfect Patient Pathway Test Bed Overview Report can be found here.
The Perfect Patient Pathway Test Bed Evaluation Report can be found here.
To view the Perfect Patient Pathway Test Bed project films visit YouTube, here.
The Digital Care Home Evaluation Report can be found here..
Download the following Perfect Patient Pathway case studies here:
- Digital care home project
- Asthma – exploring self-management
- Strength and balance
- Digital health training: supporting patients to use technology to manager their health